Health Insurance Glossary: 20 Key Terms You Should Know
Understanding health insurance can be challenging, especially with the complex terminology used throughout policies and medical documents. If you’re shopping for a health insurance plan or trying to make the most of your existing coverage, it’s essential to understand the key terms that frequently appear in policy descriptions and provider communications. A clear grasp of these health insurance terms will not only help you make more informed decisions but also empower you to confidently manage your healthcare expenses. In this health insurance glossary, we’ll break down 20 of the most important terms every policyholder should know.
When exploring any health plan, one of the first concepts you’ll encounter is the premium—the amount you pay regularly (monthly, quarterly, or annually) to maintain your insurance coverage. Unlike other costs, this is owed whether or not you use medical services. Closely related to the premium is the deductible, which is the amount you must pay out-of-pocket for healthcare services before your insurance begins to share the cost. Plans with lower premiums often have higher deductibles, and vice versa, so balancing these two factors based on your expected healthcare needs is crucial.
Once your deductible is met, your insurance typically begins cost-sharing, and that’s where co-pays and co-insurance come in. A co-pay is a fixed fee you pay for specific services, like a doctor visit or prescription. In contrast, co-insurance is a percentage of the total cost of a covered service that you’re responsible for after the deductible has been reached. For example, if your co-insurance is 20%, and a procedure costs $1,000, you would pay $200 while your insurance covers the remaining $800.
Another essential term is the out-of-pocket maximum—this is the maximum amount you will have to pay in a year for covered services. After you reach this limit, your insurance covers 100% of eligible costs for the rest of the plan year. This cap includes your deductible, co-pays, and co-insurance, but not your premium. Understanding this term is critical for budgeting and avoiding unexpected financial strain in the event of major medical issues.
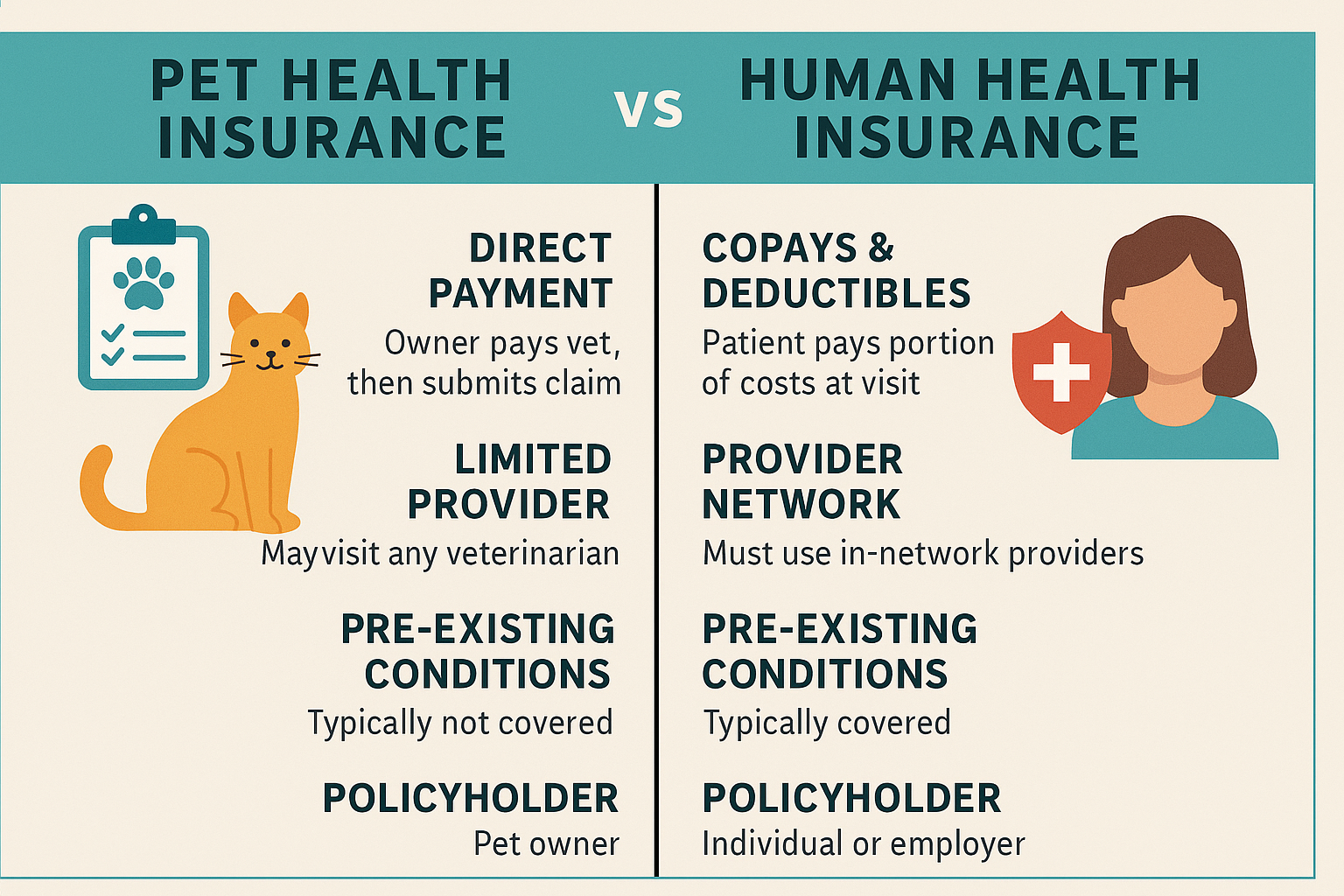
The provider network is another cornerstone of any health insurance plan. Health insurance companies contract with specific doctors, hospitals, and clinics—called in-network providers—to deliver services at pre-negotiated rates. Using out-of-network providers can result in higher out-of-pocket costs or no coverage at all, depending on your plan. Therefore, it’s important to confirm that your preferred healthcare providers are within your insurer’s network before receiving care.
A primary care physician (PCP) serves as your main healthcare provider and may be required by certain plans such as HMOs (Health Maintenance Organizations). In contrast, plans like PPOs (Preferred Provider Organizations) allow more flexibility in seeing specialists without referrals. If you need specialized care, your PCP may issue a referral, which is often required for insurance to cover the visit.
Formulary refers to the list of prescription drugs covered by your health insurance. Drugs are usually grouped into tiers that determine your cost. If your medication isn’t on the formulary, you may face higher costs or need special approval, known as a prior authorization, to obtain coverage. Some drugs may also be subject to step therapy, a process where you must try lower-cost medications first before your plan will cover more expensive alternatives.
Pre-existing conditions are health issues you had before your insurance coverage began. Thanks to the Affordable Care Act, insurers can no longer deny coverage or charge higher premiums based on these conditions. However, it’s still wise to verify how a plan manages care for ongoing conditions.
Another term you might encounter is Explanation of Benefits (EOB)—this is not a bill but a statement sent by your insurance company after you receive care, outlining what was covered, what the provider charged, what the insurer paid, and what you may owe.
Also important are Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs), which let you set aside pre-tax money to pay for qualified medical expenses. These accounts can help reduce your taxable income while offering a way to cover deductibles and other out-of-pocket costs.
In today’s digital age, many insurers offer telehealth options, allowing you to consult with doctors via video or phone for minor conditions, mental health care, and follow-up visits. This modern approach is often faster and more affordable than traditional in-person visits.
By learning these terms, you can better understand your policy, reduce confusion, and make more confident healthcare choices. Whether you’re comparing plans, disputing a claim, or preparing for an upcoming procedure, being fluent in health insurance terminology will help you navigate the system with clarity and control. Make sure to revisit this glossary regularly, especially during open enrollment periods or when switching plans, to ensure you’re always equipped with the knowledge needed to protect your health and your finances.