Health Insurance for Maternity and Family Planning
Navigating health insurance options for maternity and family planning has become increasingly important in 2025 as more individuals and couples seek comprehensive coverage to support their reproductive choices and prenatal care. Health insurance plays a crucial role in reducing the financial burden associated with pregnancy, childbirth, fertility treatments, and postnatal care. Whether you are planning to start a family, already expecting, or exploring fertility options, understanding how your health insurance policy addresses these needs is essential to ensure proper care and avoid unexpected costs. With the continued evolution of healthcare policies and technology, knowing what to look for in a maternity and family planning insurance plan is more critical than ever.
Most standard health insurance plans under the Affordable Care Act (ACA) are required to include maternity and newborn care as essential health benefits. This means that both individual and employer-sponsored insurance plans must cover prenatal visits, labor and delivery, and postnatal care. However, the depth and quality of coverage can vary significantly based on the insurer, the type of plan (HMO, PPO, or high-deductible), and your location. Comprehensive maternity insurance typically includes coverage for ultrasounds, screening tests, hospital stays, epidurals, C-sections, and newborn check-ups. Some plans may even provide lactation support and postpartum mental health services, which are essential for new mothers.
Family planning coverage extends beyond maternity to include birth control, sterilization procedures, and counseling. Under federal guidelines, most ACA-compliant plans cover FDA-approved contraceptive methods without charging a co-payment or coinsurance, even if the deductible hasn’t been met. This provision empowers individuals to make informed decisions about when and how to start a family. It’s also worth noting that many insurance providers are now expanding benefits to include infertility treatments, such as intrauterine insemination (IUI), in vitro fertilization (IVF), and fertility preservation services, though coverage varies widely and may require specific rider policies or prior authorization.
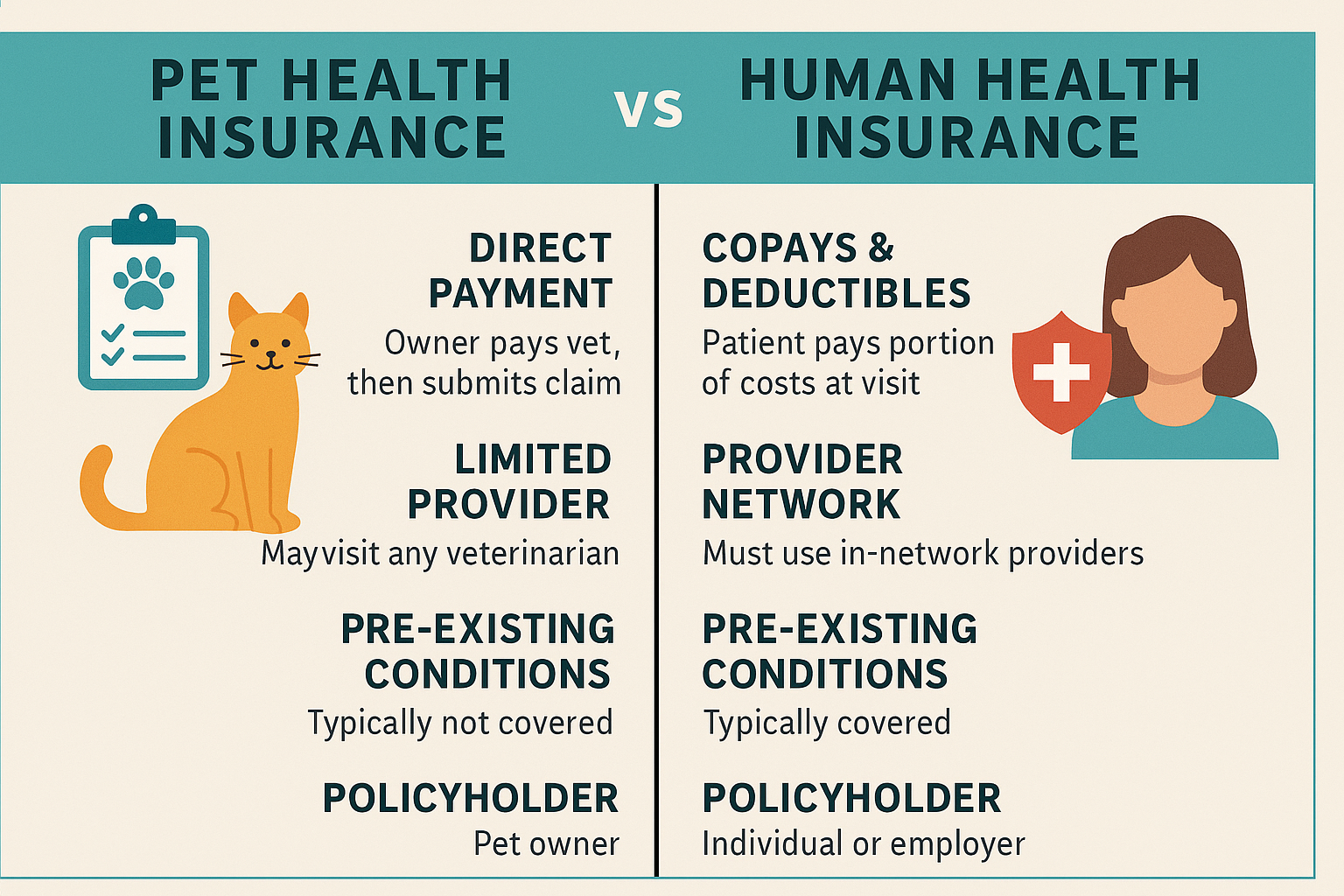
When evaluating a health insurance plan for maternity and family planning, it’s important to look at more than just the premium cost. Pay close attention to the deductible, out-of-pocket maximums, hospital network, and in-network provider availability. Maternity-related hospital stays and procedures can quickly exceed several thousand dollars, so selecting a plan with lower out-of-pocket expenses can be financially beneficial in the long run. Additionally, confirming that your preferred OB-GYN or birthing center is in-network can prevent substantial surprise billing.
Telehealth is also emerging as a powerful tool in maternal care, offering convenient access to prenatal consultations, birth planning sessions, and postpartum therapy. Many insurance providers now cover virtual visits as part of their maternity and family planning benefits, which can save time and reduce exposure to healthcare settings during sensitive stages of pregnancy. This added flexibility supports more inclusive and accessible care, especially in rural areas or for individuals with limited mobility or transportation options.
In conclusion, choosing the right health insurance plan for maternity and family planning in 2025 requires a thorough understanding of what’s covered, the potential costs, and the flexibility offered through modern care delivery models like telehealth. With rising healthcare expenses and evolving family needs, comprehensive coverage ensures that you’re supported at every step of your journey—from planning and conception to delivery and postnatal care. Investing time in comparing plans, checking benefits, and understanding your legal rights can provide peace of mind and allow you to focus on what truly matters: building a healthy and supported family.