Health Insurance and Mental Health: What’s Covered?
In 2025, the conversation around mental health has reached new heights, with growing recognition of its vital role in overall well-being. As a result, health insurance providers are increasingly integrating comprehensive mental health coverage into their plans. Understanding what is covered under your health insurance when it comes to mental health services is crucial for accessing the care you need without financial strain. This article explores how mental health coverage works, what services are typically included, and how to ensure you’re getting the most from your plan. With mental health becoming a priority in both public and private healthcare, navigating your insurance options has never been more important.
Most modern health insurance plans, whether offered through employers, government programs like Medicaid and Medicare, or purchased through the ACA marketplace, are required to cover mental health and substance use disorder services at the same level as physical health care. This requirement, known as mental health parity, ensures that mental health conditions like depression, anxiety, bipolar disorder, and post-traumatic stress disorder (PTSD) are not treated with less importance than conditions like diabetes or heart disease. Thanks to this legislation, mental health services are not considered optional or secondary—they are essential benefits.
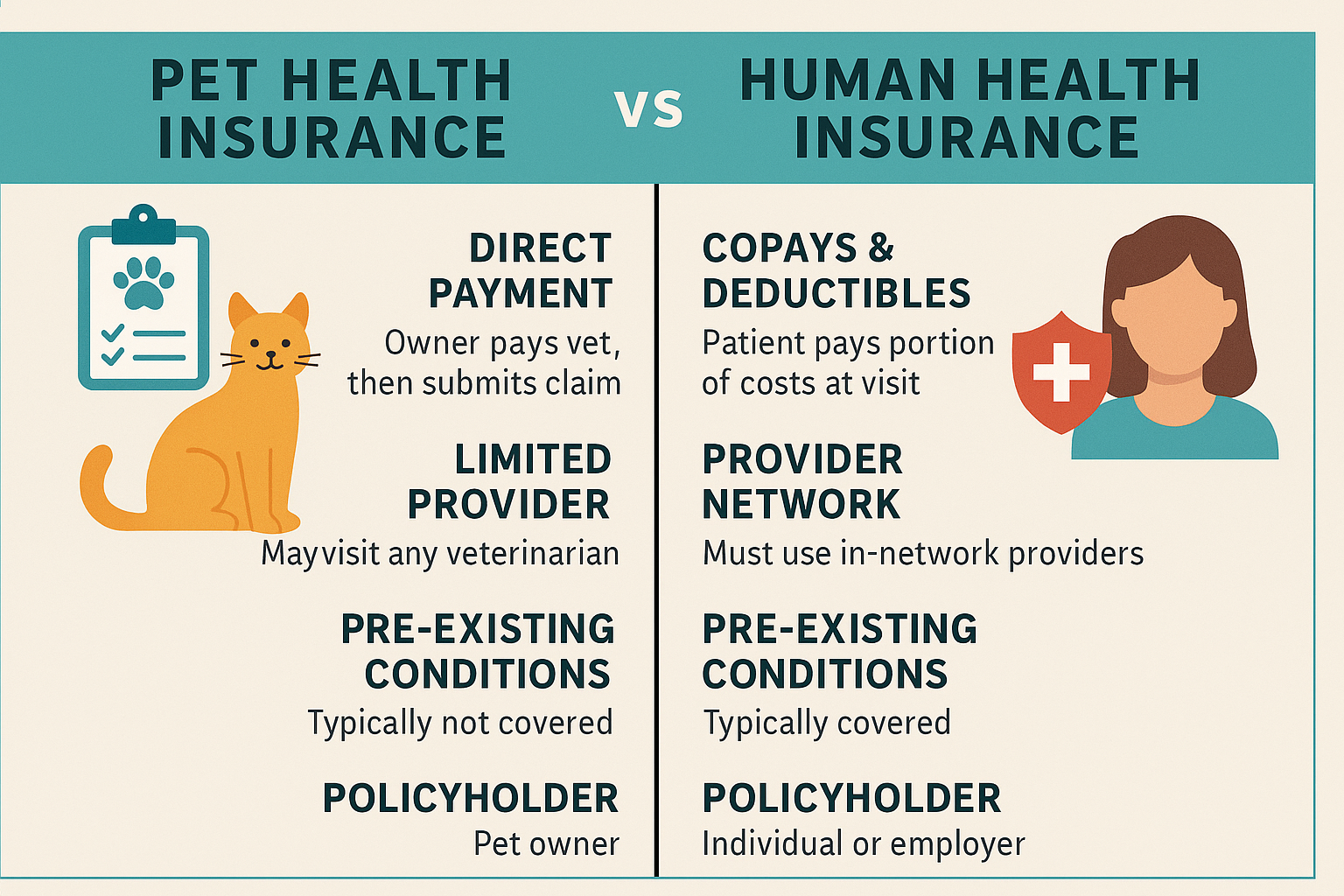
Coverage typically includes outpatient therapy, such as sessions with a psychologist, licensed therapist, or psychiatrist. These sessions may be individual, group, or family-based, depending on the needs of the patient. Many insurance plans cover a set number of therapy sessions per year or offer coverage with a copayment or coinsurance after meeting a deductible. Importantly, therapy is no longer limited to in-person visits. In response to growing demand and technological innovation, telehealth services have become widely accepted by insurers, allowing patients to receive virtual therapy sessions from the comfort of home.
In addition to outpatient care, most health insurance plans also cover inpatient mental health services for more severe conditions that require hospitalization or residential treatment. This can include stays at psychiatric facilities or mental health units within hospitals. Coverage usually extends to room and board, medication management, and intensive therapy during the patient’s stay. Preauthorization may be required for inpatient treatment, so it’s important to consult your provider and understand the criteria before seeking such services.
Prescription medications for managing mental health conditions are also widely covered under standard health insurance plans. This includes antidepressants, anti-anxiety medications, mood stabilizers, and antipsychotic drugs. Plans typically categorize these drugs into tiers with varying levels of cost-sharing, but they are required to offer at least one medication per therapeutic category. Patients may need prior authorization for certain medications, and it’s important to work closely with a healthcare provider to choose a treatment plan that fits both medically and financially.
Substance use disorder treatment is another critical area now covered by most health insurance plans. Services such as detox programs, outpatient counseling, medication-assisted treatment (MAT), and inpatient rehabilitation are considered essential benefits. With substance use disorder rates rising globally, insurance providers have expanded access to evidence-based treatments that can be life-saving for individuals battling addiction. This coverage not only promotes recovery but also prevents future medical complications, lowering long-term healthcare costs.
It’s important to note that coverage specifics can vary widely depending on the insurance provider, the type of plan, and the state or country in which you reside. Some plans may limit the number of covered sessions or require referrals from a primary care physician. To make the most of your mental health benefits, it’s essential to verify what services are covered, what providers are in-network, and whether preauthorization is needed for certain types of care. Most insurance companies offer online portals and customer service support to help members navigate their benefits.
In conclusion, mental health coverage in health insurance plans has significantly improved, offering broader access to vital services in 2025 than ever before. From therapy and psychiatric care to medication and addiction treatment, most modern insurance plans include comprehensive mental health benefits. As awareness continues to grow, mental health care is no longer a luxury—it’s a necessity, and your insurance should reflect that. Understanding your plan’s mental health benefits empowers you to seek timely, effective care that supports both your mind and body, improving your quality of life and overall health.