Common Reasons Health Insurance Claims Get Denied
Understanding the common reasons why health insurance claims get denied is critical in 2025, especially as healthcare costs continue to rise and policyholders seek to maximize their benefits. A denied claim can lead to unexpected out-of-pocket expenses, administrative stress, and delays in care. By recognizing the typical issues that trigger claim rejections, policyholders can take proactive steps to ensure smoother processing and better reimbursement outcomes. Most health insurance denials result not from the treatment itself, but from avoidable errors, incomplete documentation, or misunderstandings between the policyholder, provider, and insurer.
One of the most frequent causes of claim denial is submitting incomplete or inaccurate information. Insurance companies require precise details including patient demographics, policy numbers, diagnosis codes (ICD-10), and procedure codes (CPT/HCPCS). If any of this data is missing or incorrect, the insurer may automatically reject the claim. This issue often arises when forms are filled out in a rush or submitted without double-checking, which is why careful review before submission is essential. Additionally, claims must often be filed within a specific timeframe, usually between 90 and 180 days from the date of service, and missing that deadline can result in automatic denial.
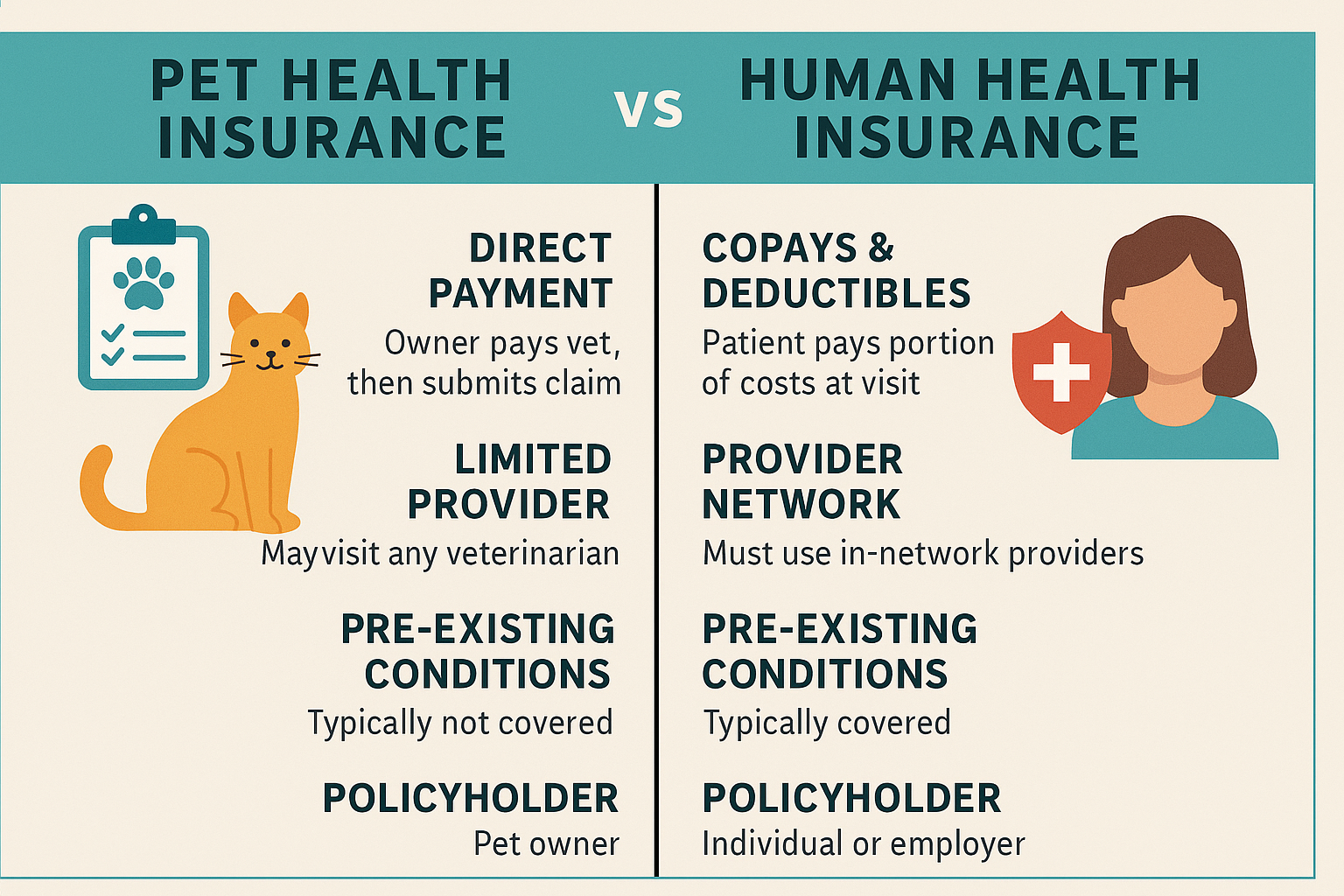
Another common reason for denied health insurance claims is seeking care from an out-of-network provider without prior authorization. While many policies include coverage for emergency services regardless of provider, non-emergency care must typically be rendered by an in-network provider to be covered fully. If a patient visits a doctor, specialist, or facility that is not within their insurer’s preferred provider network, the claim may be partially or entirely denied unless pre-authorization was obtained. In 2025, many insurers offer mobile apps or online directories to help consumers verify provider status before making an appointment, which can help prevent costly missteps.
Medical necessity is another key factor. Insurers often deny claims for treatments they deem not medically necessary or not aligned with the plan’s coverage terms. This is particularly common for procedures classified as experimental, elective, cosmetic, or lacking adequate documentation. For example, a claim for advanced imaging like an MRI may be denied if the insurer believes that a less expensive test, such as an X-ray, would have been sufficient. To avoid this, it’s vital to ensure that your provider submits detailed clinical notes and justification showing why the treatment was required based on your condition.
Failure to obtain pre-authorization or a referral can also lead to claim denials. Certain tests, procedures, and specialist visits require the insurance company’s approval before they’re performed. If a patient skips this step or if the provider fails to submit the necessary paperwork in advance, the claim may not be honored. This scenario is common with surgeries, mental health services, and high-cost diagnostics. Staying informed about your plan’s prior authorization requirements and working closely with your provider to obtain them can make a significant difference in avoiding denied claims.
In some cases, claims are denied due to coverage exclusions or limitations clearly outlined in the policy. Every health insurance plan includes a summary of benefits that specifies what is and isn’t covered. Services like alternative therapies, cosmetic procedures, or experimental treatments may be excluded entirely. If a policyholder receives such a service and files a claim without verifying coverage, the insurer is likely to deny it outright. Reviewing your plan documents regularly and contacting your insurer with questions about coverage can help prevent these types of denials.
Lastly, administrative errors on the part of either the healthcare provider or the insurance company can also result in claim denials. These errors may include duplicate billing, coding mistakes, or mismatched patient records. Though these issues are not the policyholder’s fault, it’s crucial to review the Explanation of Benefits (EOB) and medical bills closely to identify any inconsistencies. In many cases, denied claims due to administrative errors can be resolved quickly through a corrected resubmission or appeal.
In conclusion, while claim denials are a frustrating part of navigating health insurance, most are preventable. By understanding the most common reasons claims are denied—such as incomplete information, out-of-network care, lack of medical necessity, missing pre-authorization, policy exclusions, and administrative mistakes—policyholders can take proactive steps to ensure claims are processed correctly and efficiently. In 2025, with digital tools and more transparent provider networks, consumers are empowered like never before to avoid costly claim errors and receive the benefits they’re entitled to under their health insurance plans.