What Does “Out-of-Network” Mean and How Much Does It Cost?
In the complex world of health insurance, the term “out-of-network” is one that policyholders should fully understand before seeking medical care. As we move through 2025, knowing whether your provider is in-network or out-of-network can significantly impact your healthcare costs and access to care. The difference between these two terms often determines not only how much you will pay for a doctor’s visit or procedure but whether your insurance will cover it at all. With insurance plans becoming increasingly complex, grasping the implications of out-of-network care is essential for anyone looking to avoid surprise medical bills and ensure they are making the most of their coverage.
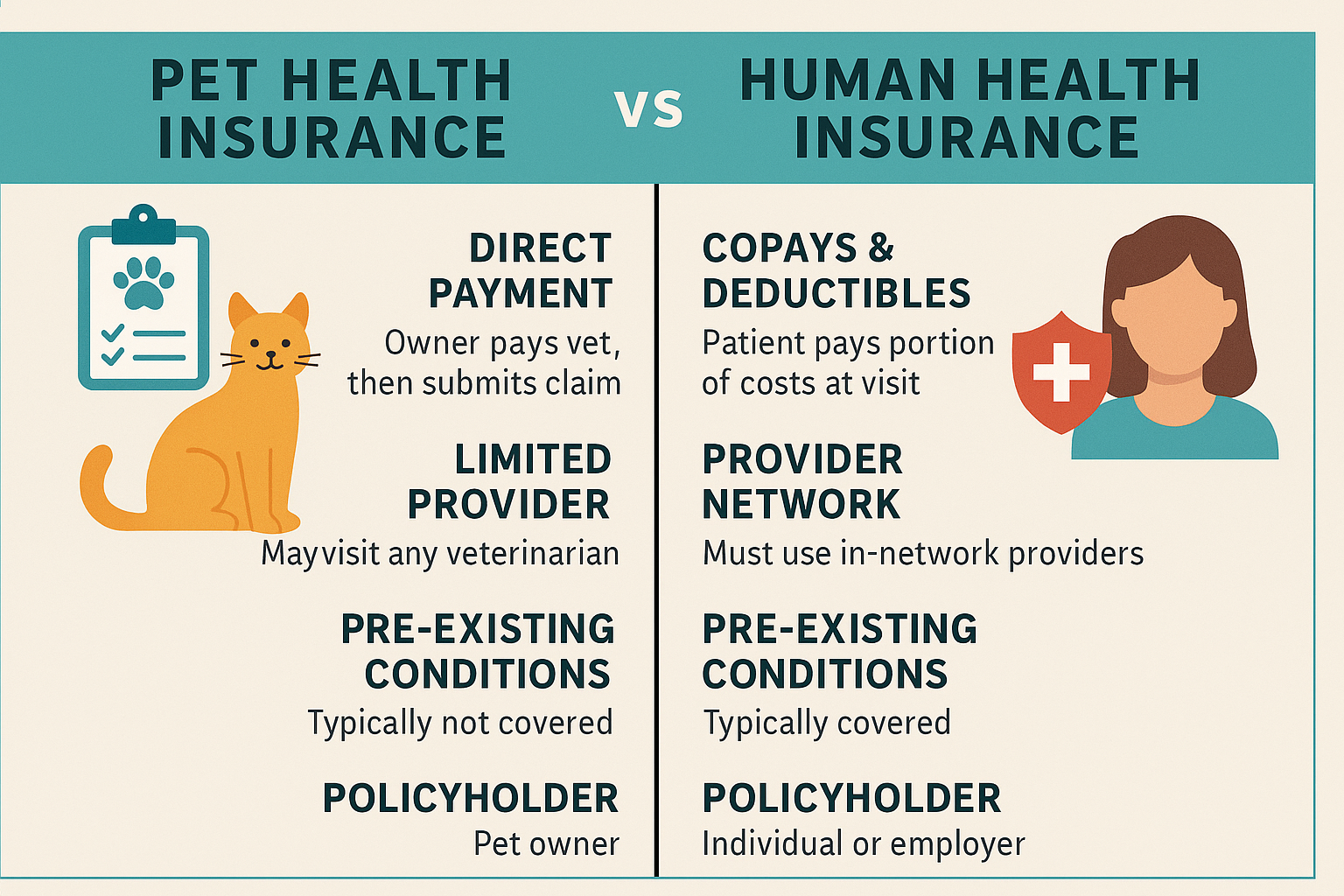
In basic terms, “out-of-network” refers to any healthcare provider, hospital, clinic, or facility that does not have a negotiated contract with your health insurance company. Most insurance plans have a list of approved providers known as the “network.” These in-network providers agree to accept discounted rates for services, which benefits both the insurer and the patient by keeping costs lower. When you seek care outside of this network, those same discounts typically do not apply. As a result, you may be responsible for a much larger share of the bill—or even the full amount—depending on the terms of your policy.
The cost of out-of-network care can be significant. While some insurance plans, such as Preferred Provider Organizations (PPOs), may offer partial coverage for out-of-network services, many plans like Health Maintenance Organizations (HMOs) provide little to no reimbursement unless it’s an emergency. This means patients could face much higher deductibles, higher coinsurance rates, and larger out-of-pocket maximums. For example, an in-network hospital visit might require a 20% coinsurance payment after meeting a deductible, but the same visit to an out-of-network hospital could result in a 40% or 50% coinsurance—or worse, complete denial of coverage. Moreover, out-of-network providers are not obligated to limit their charges, which can lead to “balance billing,” where the patient is billed for the difference between what the provider charges and what the insurance pays.
Another factor that drives up out-of-network costs is lack of transparency. Patients often discover too late that a particular lab, anesthesiologist, or specialist involved in their care is not in-network, even if the primary hospital or surgeon is. This is why it’s critical in 2025 to verify all providers involved in your care ahead of time. Many insurance companies now offer online tools and mobile apps that allow policyholders to search for in-network doctors and facilities. Taking advantage of these tools can help consumers avoid unexpected expenses and make more informed decisions.
In emergency situations, most health insurance plans are required to cover care regardless of network status. However, follow-up treatments and rehabilitation services may not be covered if they are out-of-network. It is important to contact your insurance company immediately after an emergency visit to ensure that any continued care is arranged within the network whenever possible. Additionally, some states and countries have implemented laws to protect consumers from surprise out-of-network billing, especially in emergencies, but these laws vary and may not apply to every scenario.
For patients who regularly travel, live in rural areas, or require access to a wide range of specialists, choosing a health insurance plan with out-of-network benefits, like a PPO or POS (Point of Service) plan, may be worth the additional premium. These plans offer more flexibility and can provide partial reimbursement for out-of-network care, helping to reduce financial strain. However, for those on tighter budgets or with simpler healthcare needs, sticking to in-network providers under an HMO or EPO (Exclusive Provider Organization) plan is usually more cost-effective.
Ultimately, understanding what “out-of-network” means and how it affects your health insurance coverage is essential to avoiding high medical bills and maximizing the value of your plan. As the healthcare landscape in 2025 becomes more consumer-driven, patients must take an active role in managing their coverage. Always read your policy’s fine print, know your network boundaries, and contact your insurer when in doubt. Doing so can save you hundreds or even thousands of dollars annually while ensuring that you receive timely and appropriate care.